Noticing blood in your stool can be alarming. While it may be caused by something as minor as hemorrhoids, it can also be an early warning sign of colorectal cancer. Understanding the causes, symptoms, and when to seek help is vital for early detection and successful treatment.
Understanding Blood in Stool
Bleeding in stool or rectal bleeding may be manifested in several different ways:
- Vibrant red blood on toilet paper or in the toilet
- Dark red or maroon-colored stool
- Black, tarry stools (melena)
Each form of bleeding could signal a different gastrointestinal (GI) tract issue. Vibrant red tends to suggest lower GI tract problems, and darker blood can come from the upper GI tract.
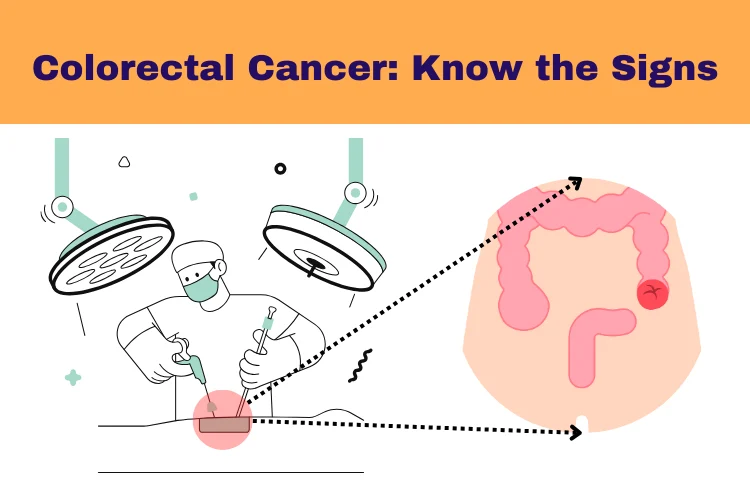
Is Blood in Stool a Symptom of Colorectal Cancer?
Yes, blood in stool can be a symptom of colorectal cancer, especially when it persists or is accompanied by other changes in bowel habits. Colorectal cancer often begins as benign polyps that may bleed as they grow.
Common Signs of Colorectal Cancer
In addition to blood in the stool, other warning signs include:
- A change in bowel habits (diarrhea, constipation, or narrow stools)
- Unexplained weight loss
- Persistent abdominal discomfort (cramping or pain)
- A feeling of incomplete evacuation
- Fatigue or weakness
- Iron-deficiency anemia
These symptoms may develop gradually, and early-stage colorectal cancer may show no symptoms at all. That’s why routine screenings are crucial.
Learn more about Early Signs of Colon Cancer
Other Causes of Blood in Stool
While colorectal cancer is a serious concern, other non-cancerous conditions can also cause rectal bleeding:
1. Hemorrhoids
Swollen blood vessels in the rectum or anus that can cause bright red bleeding.
2. Anal Fissures
Small tears in the lining of the anus, usually from straining during bowel movements.
3. Diverticulosis
Pouches in the colon wall that can become inflamed and bleed.
4. Inflammatory Bowel Disease (IBD)
Conditions like Crohn’s disease and ulcerative colitis can cause bleeding and inflammation.
5. Polyps
Benign growths in the colon that may bleed. Some can turn cancerous if not removed.
6. Gastrointestinal Infections
Bacterial or viral infections can irritate the lining of the GI tract and lead to bloody diarrhea.
When to See a Doctor
Not every occurrence of blood in stool is caused by cancer, but it cannot be dismissed. Visit your doctor if you experience:
- Recurring or ongoing blood in stool
- Black or tarry stools
- Blood with abdominal pain
- Unintentional weight loss
- Weakness or shortness of breath
Your physician may order such tests as a colonoscopy, stool tests, or imaging to identify the reason.
Screening and Early Detection
Routine colorectal cancer screening is the best way to detect cancer early—even before symptoms appear. Common screening methods include:
- Colonoscopy
- Fecal occult blood test (FOBT)
- Fecal immunochemical test (FIT)
- CT colonography
Screenings are typically recommended starting at age 45 for average-risk individuals. Those with a family history or other risk factors may need to start earlier.
Reducing Your Risk of Colorectal Cancer
You can reduce your risk of colorectal cancer by changing your lifestyle:
- Eat a high-fiber diet: Include whole grains, fruits, and vegetables.
- Don’t overdo red and processed meats: These are associated with increased cancer risk.
- Exercise daily: Aim for at least 30 minutes of exercise most days.
- Quit smoking: Smoking raises the risk of colorectal cancer.
- Don’t overdrink alcohol: Excessive drinking is a contributing factor.
FAQs
1. Is blood in stool always a sign of colorectal cancer?
No, it can result from hemorrhoids, fissures, or infections, but should always be evaluated.
2. What does colon cancer bleeding look like?
It can appear as bright red blood, maroon stools, or black tarry stools.
3. How is colorectal cancer diagnosed?
Through colonoscopy, biopsy, and imaging tests after symptoms or screening alerts.
4. Can polyps cause blood in stool?
Yes, some polyps bleed and can develop into cancer if not removed.
5. When should I worry about blood in my stool?
If it’s persistent, accompanied by other symptoms, or you’re over 45, see a doctor.
6. Can diet affect colorectal cancer risk?
Yes. Diets high in fiber and low in processed meat help reduce risk.
Conclusion
Although blood in the stool may have many causes, it must not be ignored, particularly if recurring or accompanied by other symptoms. Early diagnosis of colorectal cancer significantly enhances recovery, so speak to a health professional if you’re noticing anything unusual.
Don’t ignore rectal bleeding—get checked early for peace of mind and better health.